
Visual Acquity - Always first check vision ( Each eye separately , for near and far)
Pinhole test if vision is reduced
Visual Field (confrontation Method)
Color Vision Ishihara Chart,Friends chart
General examination for ptosis, proptosis,external deformity, head Posture etc
Evert eyelids if patient complains of irritation
Check anterior chamber depth
Check pupillary reaction (direct, consensual and RAPD)
Check for any lens opacity
Fundoscopy for macula and optic disc
Check IOP in every patient above 35 years of age, by both digital method and tonometer
Regurgitation test if patient complains of watering
Check IOP in every patient above 35 years of age, by both digital method and tonometer
Regurgitation test if patient complains of watering
Ocular movement ( make "H" or "X") and cover-uncover test if patient complains of diplopia/strabismus
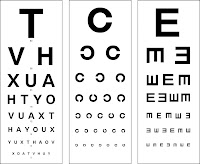 |
| Standard Snells Char |
The Ocular Examination for PG trainees:
Visual Acuity - Distance
Colour Vision
Visual Fields
Pupils
Anterior Chamber Depth
Extraocular Muscles
Alignment
Movement
• Cranial Nerve III – superior rectus, medial rectus, inferior rectus, inferior oblique
• Cranial Nerve IV – superior oblique
• Cranial Nerve VI – lateral rectus
External Examination
• the four L’s
lymph nodes (preauricular, submandibular)
lids
lashes
lacrimal system
Slit-Lamp Examination
• systematically examine all structures of the anterior segment and anterior vitreous.
Lids (including upper lid eversion if necessary), lashes, and lacrimal system
conjunctiva and sclera
cornea
Iris
Anterior chamber (for depth, cells, and flare)
Lens
Anterior vitreous
Tonometry
Ophthalmoscopy/Fundoscopy
• contraindications to pupillary dilatation:
shallow anterior chamber
Iris-supported anterior chamber lens implant
potential neurologic abnormality requiring pupil evaluation
use caution with cardiovascular disease - mydriatics may cause tachycardia
Must do things for eye examination
1. introduce yourself
2. take consent for examination
3. understand the question/scenario, if in doubt ask the examiner
4. record visual acuity for far and near with and with out glasses and also in the end do binocular visual acuity,
Ask for vision chart, if not available then do gross vision
ALWAYS ONE EYE AT ONE TIME, ASK THE PATIENT TO COVER OTHER EYE WITH PALM OF HAND
if the vision is less than 6/60 the take the patient closer to the chart by one meter up to 5 meters
if he still cannot read the big letter then do finger count at 3, 2, 1 foot,
if he still cannot count the fingers do hand movements at 6 inches, if the patient does not respond do perception of light
5. do colour vision testing
6. inspect for any eyebrow/ eyelid abnormality evert both eyelids
7. do oblique penlight examination of anterior segment
8. do light reflex, ask the patient to look at a distant object straight ahead then bring light obliquely (45 degrees angle from the temporal side into the pupil on to the retina briskly
9 check the depth of anterior chamber by observing iris shadow from front and throwing light from the temporal side in the pupillary plane
10. do consensual light reflex
11. do swinging light reflex if asked or there is any abnormality in light reflex
12.check IOP, first ask the patient to look downwards and then palpate by index fingers of both hand and stablize hand via middle fingers resting on forehead, do fluctuation test above the tarsal plate ie 10 mm above eyelid margin
13do regurgitation test by asking the the patient to look upwards then press just medial to medial canthus and observer the punctii for any reflux
if the patient complains of epiphora first examine lid for entropion/ectropion. inspect the punctii then do regurgitation test and then do gross nasal exam and also check the seventh cranial nerve function
14. ocular movements examination. be seated in front of the patient at his level and then ask the patient to fixate on you finger with both eyes and follow it in a wide H pattern extent your arms to about 2-3 feet from the mid line
15 do visual fields by confrontation method be seated in front of the patient at his level, ask the patient to close one eye, you should also close your facing eye, then bring you moving finger from the extreme periphery exactly in the middle plane between you and the patient to the center until the patient sees your finger without moving his eyes or head repeat this in all four quadrants
16. do any other test as required in the scenerio
17 DURING EXAMINATION REMEMBER THE POSITIVE FINDING AND MAKE A DIFFERENTIAL DIAGNOSIS
17 thank the patient and the examiner
REMEMBER 20-25 % MARKS FOR GREETING CONSENT AND THANKS
FOR PASSING DO VISUAL ACUITY AND PUPIL LIGHT REFLEX VERY VERY CAREFULLY AND CORECTLY
PRACTICE AGAIN ON PATIENTS AND FELLOW STUDENTS
An Ophthalmologist Must Memorize The following Facts:
- Steroids are contraindicated in corneal ulcer
- Atropine is contraindicated in narrow angle glaucoma
- Steroids are indicated in uveitis
- Atropine is indicated in uveitis
- Never dilate a patent with narrow angle
- Never prescribe local anesthetics for corneal ulcer
- There are no symptoms of POAG
